How To Lose Weight With Lipedema – A Disease Causing Disfiguring Fat Deposits
Lipedema is a condition affecting 11% of women globally, with an estimated 70 million in the US and up to 350 million worldwide. It's characterized by the chronic and progressive buildup of fat tissue and lymph, resulting in a disproportionate enlargement of the upper and or lower limbs in relation to the upper part of the body. The feet and hands are typically not affected. Seeking treatment from a holistic functional medicine practitioner can offer a comprehensive approach to managing symptoms.
Despite its prevalence, lipedema often goes undiagnosed due to the absence of standardized diagnostic tests. Unlike obesity, it's not caused by excess calorie intake, making it crucial to distinguish between the two conditions. A key point of distinction is that lipedema fat is resistant to reduction through traditional methods like rigorous diet and strenuous exercise. Incorporating holistic medicine into your approach can target the underlying factors contributing to lipedema.
Symptoms of Lipedema
Disproportionate body fat distribution, commonly in the legs
Symmetrical swelling in the legs, thighs, hips, and sometimes the arms, often with a "cuff" above the ankles
No or limited response to weight loss in affected areas
Swollen or “marbled” appearance of the skin
Limb Pain
Unexplained Bruising
Increased sensitivity to touch
Discomfort
Tenderness
In later stages:
High-intensity pain
Limited mobility
Severe varicose vein issues including bulging varicose veins
Venous hypertension
Poor wound healing
Root Causes
Excessive interstitial fluid accumulation
Fat cell increase (number + size)
Excessive collagen deposition leading to fibrosis
Lowered oxygen supply due to fat cells blocking circulation.
Lymphatic dysfunction
Altered lipid panels (Elevated LDL, Total Cholesterol, Triglycerides).
Genetic predisposition
Vascular dysfunction
Lipedema vs. Lymphedema
Unlike lymphedema, which often manifests in a single limb and involves fluctuating swelling associated with a dysfunctional lymphatic system, lipedema symmetrically affects the body. Both conditions can coexist. Lymphedema results from a blockage or insufficiency in the lymphatic system, hindering proper fluid drainage. Primary lymphedema may have a genetic basis, while secondary lymphedema can arise from factors such as surgery, radiation, infection, or injury.
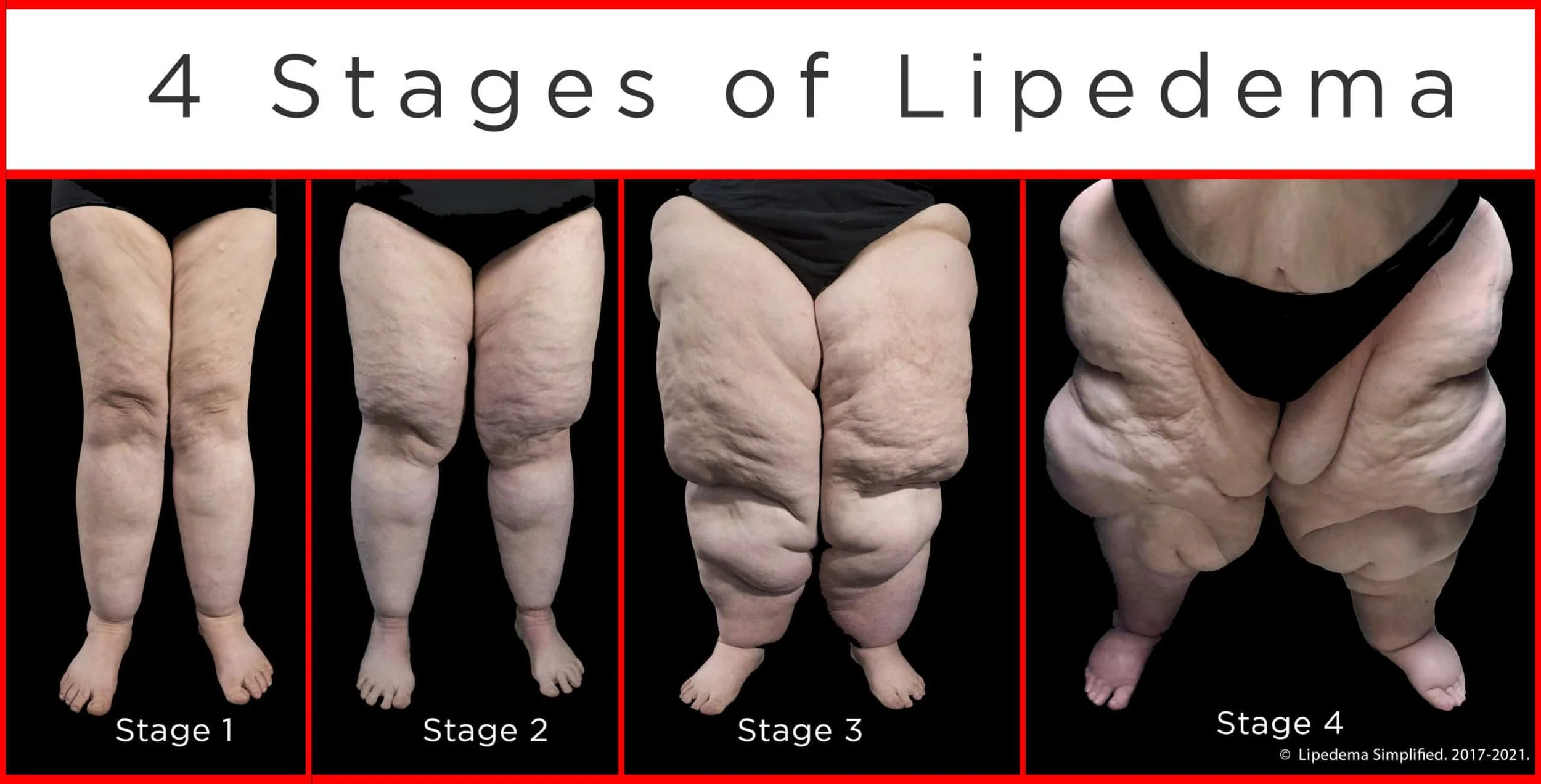
Stages of Lipedema
The condition typically advances through various stages, each with distinct characteristics:
Stage 1:
Appearance: Skin appears normal, but there is soft, palpable fat underneath.
Symptoms: Heaviness, discomfort, sudden fat build-up in the lower body (buttocks, hips, thighs, calves), aching legs, and inflammatory pain.
Stage 2:
Appearance: Uneven skin resembling a mattress or orange peel. Fat becomes fibrotic, and nodular, forming lipomas.
Symptoms: Increased discomfort, weight gain, and sensitivity in affected areas.
Stage 3:
Appearance: Hardening and thickening of the subcutaneous tissue. Large fat lobules form around the thighs, knees, and sometimes lower legs. Skin texture becomes more uneven, accumulating in hips, buttocks, thighs, and calves.
Symptoms: Mobility affected, increased pain, higher risk of bruising.
Stage 4:
Appearance: Often characterized by lymphedema, significant swelling due to lymphatic dysfunction.
Symptoms: Increased pain, mobility issues, frequent infections
The Lipedema-Inflammation-Connection
The difficulty in losing Lipedema fat is attributed to inflammation and fibrosis within the tissue. Chronic inflammation does not only lead to insulin resistance and the development of metabolic disorders (hello weight gain), but it also hinders the lymphatic system, responsible for clearing fluid and waste from tissues. As the lymphatic system slows down, fluid accumulates, creating an environment in which fat cells thrive. This stagnant fluid, laden with waste material and nutrients, becomes a breeding ground for fat cell growth in both size and number. The hypoxic (low-oxygen) conditions resulting from this growth lead to damaged cells with altered metabolism and mitochondrial impairment. Subsequently, dying cells trigger an immune response, where immune cells act as "Pacman" to clear debris.
Fat tissue is under constant pressure to regulate fluid balance. An ongoing influx of fluid into fat tissue necessitates efficient removal through both the venous and the lymphatic system. The collaboration between these systems is crucial for the continual removal of fluid. If these systems are defective, swelling becomes an inevitable consequence.
The inflammatory cascade induces a process known as microangiopathy, which increases fragility and permeability in blood vessels. Low oxygen levels prompt the formation of additional small blood vessels to enhance oxygen supply, overwhelming lymphatic pumps due to increased fluid influx without a corresponding increase in outflow. Ultimately, this process contributes to the development of lymphedema in many patients with lipedema. The painful abnormal fat in lipedema patients is thought to be a result of low oxygen and inflammation.
The Lipedema-Gut -Estrogen-Connection
Since half of the lymphatic system resides in the gut, lipedema is closely linked to gut health. Additionally, more than half of all lymph, especially from the liver, originates in the gut. The gut microbiome plays a crucial role in various bodily functions. It regulates metabolism, energy levels, food absorption, and even estrogen levels. Abnormal estrogen levels are often associated with dysbiosis.
Gut dysbiosis, especially an abundance of gram-negative bacteria, is a significant factor in Lipedema. Gram-negative bacteria have a resilient outer shell composed of endotoxins or Lipopolysaccharides (LPS). These tough particles persist even after bacteria die, entering the gut, and bloodstream, and triggering the immune system. Elevated endotoxin levels stop or slow the lymphatic pumping action and cause leakage. Fat cells notably expand when exposed to lymphatic fluid. Additionally, the lymph leakage exacerbates systemic inflammation throughout the body.
Lipedema is almost exclusively found in females and primarily manifests in hormonal periods like puberty, pregnancy, or menopause, why it is thought to be estrogen-mediated. Additionally, gynecological trauma or surgery can trigger the onset of the condition. Weight loss resistance is thought to be influenced by estrogen, a hormone that plays a central role in various aspects of metabolism: it is involved in regulating the body's energy homeostasis, fat metabolism, managing food intake as well as energy consumption in the hypothalamus.
Adipose tissue expands through two main processes: adipocyte hypertrophy (increase in fat-cell number) and hyperplasia (increase in fat-cell size). Some hypotheses suggest that alterations in estrogen receptors may contribute to both hyperplasia and hypertrophy of fat cells.
The Lipedema-Lymph-Liver-Connection
The liver, the largest lymph-producing organ, contributes significantly to the body's lymph production. A healthy liver generates half of the total lymph in the body. In various liver diseases, including non-alcoholic fatty liver disease, the lymph output from the liver increases. As the liver's health declines, the lymph output surges, potentially reaching six to 10 times the normal level, leading to an overflow into the central lymphatic system and potentially resulting in swelling. An unhealthy liver also contributes to issues like gut dysbiosis and abnormal bile levels, creating a vicious cycle of health challenges interconnected with Lipedema.
The Role of Extracellular Matrix, Elasticity, and Vascular Changes
Fat tissue encompasses more than adipocytes; it includes fibroblasts, stem cells, and immune cells that collectively form an extracellular matrix (ECM). This net-like structure provides shape to fat tissue and plays a crucial role in its function. Fluid, nutrients, and cells from blood vessels enter the loose connective tissue (LCT), interacting with cells and exiting along with cell waste through lymphatic vessels. LCT communicates with the body through the secretion of adipokines, facilitating flow through the binding of ECM fibers to cells and tissues.
In lipedema, damaged LCT with a clogged ECM allows lipedema tissue to spread, hindering fat loss by conventional measures. When fat tissue undergoes pathological changes, it enters a state known as adisopathy or sick fat. This condition arises when fat accumulates beyond its capacity to sustain its typical structure and function. Sick fat is characterized by the enlargement of adipocytes, inflammation, and the development of fibrosis - the precise features observed in the fat tissue of individuals with lipedema. Notably, people with lipedema exhibit dilated small vessels in lipedema LCT compared to controls, reflecting lower elasticity and potential connective tissue defects, including veins. These dilated vessels release a greater volume of fluid into the ECM over time.
The loss of elastic tissue and abnormal vasculature is proposed as another theory explaining the mechanisms of lipedema. It makes fluid transport less efficient, as the usual tension created by elastic skin, which normally applies pressure on the underlying tissue, is reduced. This tension is crucial for aiding fluid in finding its way into the lymphatic and venous systems. In the context of lipedema, the theory suggests that as adipose tissue expands, the loss of elasticity hampers the ability of lymph vessels to open under increased pressure in the extracellular matrix. This, in turn, leads to capillary leakage in the tissue, resulting in hypoxia (=lack of oxygen). Hypoxia stimulates the release of vascular endothelial growth factor (VEGF) and promotes the proliferation of stem cells within the adipose tissue.
Abnormal VEGF Signaling
VEGF, or vascular endothelial growth factor, is a crucial biological signal implicated in both Lipedema and issues with the blood system. VEGFs and their receptors play a unique role in maintaining a balance between the creation of new blood vessels and the upkeep of existing ones. Abnormal VEGF signaling grows ineffective lymphatic vessels and impairs lymphatic system function. Abnormal VEGF signaling poses a significant concern, especially in the context of cancer. Cancer cells or tumors rely on triggering abnormal blood vessel growth through the VEGF signal to sustain their growth. If they cannot establish their independent blood supply, they can only reach the size of a pinhead. However, if these cells can activate abnormal blood vessel growth through the biological signal of VEGF, they gain the ability to expand and become larger. Various factors, including obesity, cancer, physical pressure, lipedema, or a high-salt diet, contribute to the occurrence of abnormal VEGF signaling.
Living with Lipedema can be both physically painful and emotionally taxing, impacting your overall quality of life. However, there is hope for significant improvement through natural, non-surgical interventions. Disrupting the cycle of endless weight gain requires a comprehensive strategy that includes weight management, anti-inflammatory interventions, as well as addressing underlying conditions. Explore my comprehensive guide in the downloadable PDF to discover effective strategies for improving your Lipedema journey and shedding stubborn fat.
Prices are in USD - please click on the document for a detailed description.